Along with artificial intelligence, patient engagement feels like the new black in health care right now. Perhaps that’s because we’re just two weeks out from the annual HIMSS Conference which will convene thousands of health IT wonks, users and developers (I am the former), but I’ve received several reports this week speaking to health engagement and technology that are worth some trend-weaving.
As my colleague-friends Gregg Masters of Health Innovation Media (@2healthguru) and John Moore of Chilmark Research (@john_chilmark) challenged me on Twitter earlier this week: are we scaling sustained, real patient engagement and empowerment yet?
Let’s dive into the reports’ findings to divine an answer for Gregg and John.
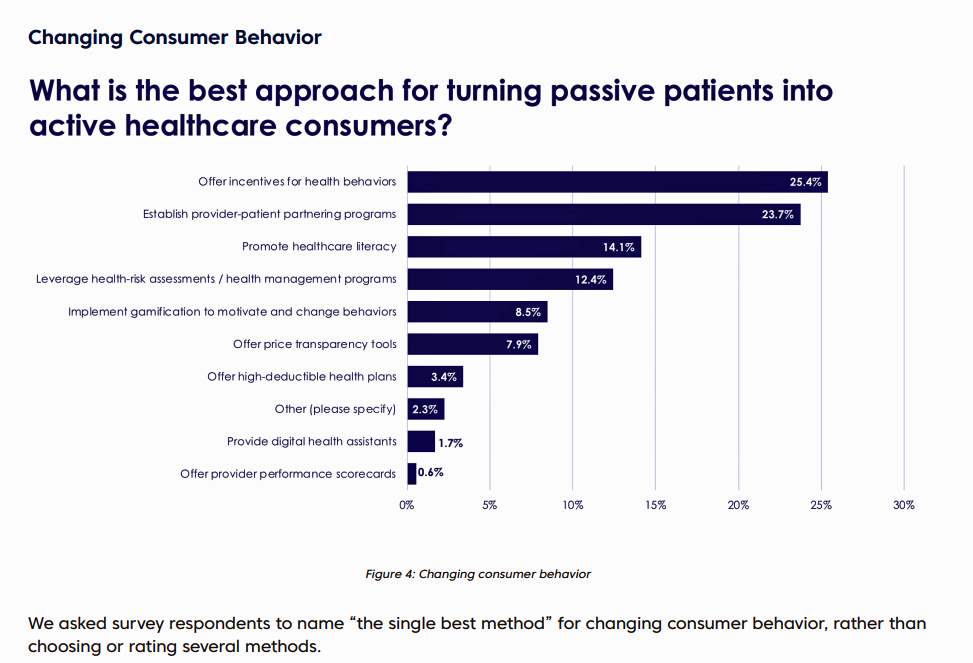 Change Healthcare published the company’s 8th Annual Industry Pulse Report, which examines key challenges facing payors and other stakeholders this year. The report analyzes results of a survey of over 2,000 Change Healthcare customers (from academia, government, technology vendors, hospitals, providers, and health plans), conducted in October-November 2017.
Change Healthcare published the company’s 8th Annual Industry Pulse Report, which examines key challenges facing payors and other stakeholders this year. The report analyzes results of a survey of over 2,000 Change Healthcare customers (from academia, government, technology vendors, hospitals, providers, and health plans), conducted in October-November 2017.
Several findings address patient and health engagement in this study, including:
- The failure of high-deductibles’ “skin-in-the-game” theory to turn patients into active health consumers
- The growth of health plans and providers integrating social determinants of health into health strategies and tactics for improving peoples’ health outcomes and engagement
- The migration of incentives from negative “sticks” to positive “carrots” along with more value-based benefit design in motivating consumer health behavior.
 One of my favorite series of papers that inform my advisory work comes from PwC on the New Health Economy, this week publishing its report on Customer experience in the New Health Economy – the data cure. A highlight of their survey found that one-half of provider executives sees customer (patient, clinician) experience as a top strategic priority over the next 5 years, and most payer execs are investing in technology to improve member experience. Remember that health insurers rank very low on consumer experience compared with retailers and grocers.
One of my favorite series of papers that inform my advisory work comes from PwC on the New Health Economy, this week publishing its report on Customer experience in the New Health Economy – the data cure. A highlight of their survey found that one-half of provider executives sees customer (patient, clinician) experience as a top strategic priority over the next 5 years, and most payer execs are investing in technology to improve member experience. Remember that health insurers rank very low on consumer experience compared with retailers and grocers.
PwC offers five pillars for healthcare stakeholders to build on to improve experience, including:
- Convenience
- Quality
- Support
- Personalization, and
- Communication.
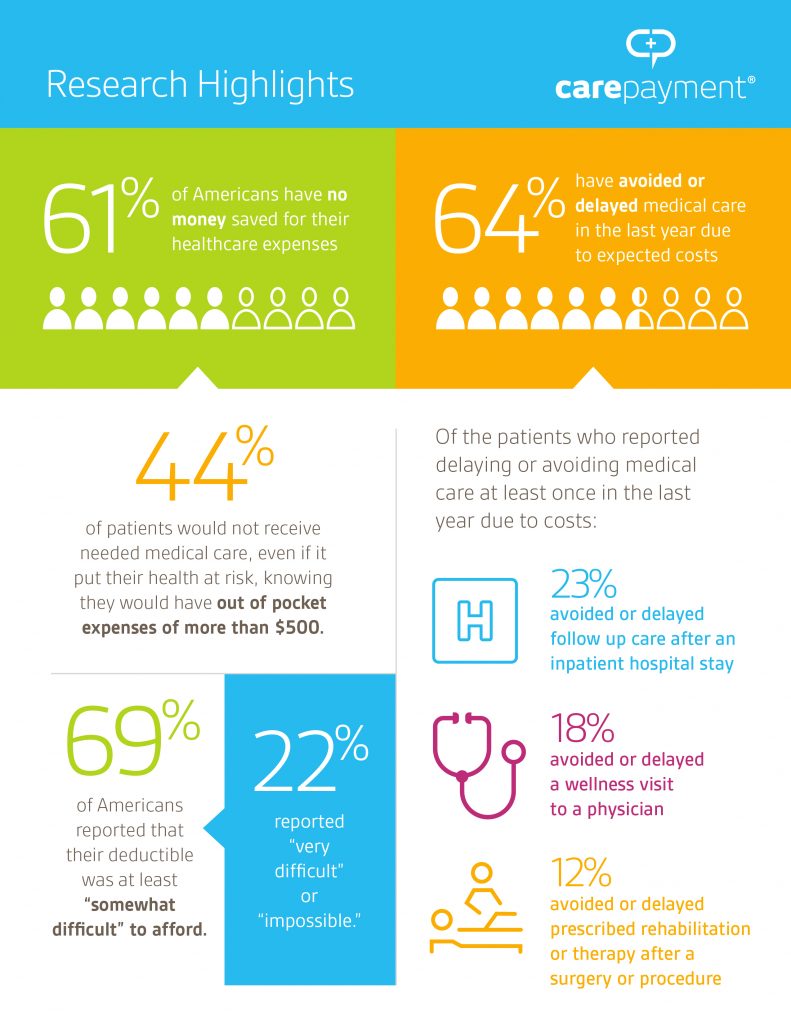 Finally, CarePayment studied the skin-in-the-game motivation for engagement, finding that 61% of patients don’t have money saved for healthcare expenses, and two-thirds of people have avoided or delayed medical care in the last year due to expected costs.
Finally, CarePayment studied the skin-in-the-game motivation for engagement, finding that 61% of patients don’t have money saved for healthcare expenses, and two-thirds of people have avoided or delayed medical care in the last year due to expected costs.
An alarming anti-engagement statistic is that 44% of the 1,000 consumers surveyed said they would not get needed medical care, even if it put their health at-risk, knowing they would have out-of-pocket expenses of $500.
The 20/20 CarePayment survey team also noted in their press release that among people who did not seek healthcare, medical debt is a growing and common problem impacting + nearly 1 in 4 Americans under 65.
The CarePayment poll was conducted in November-December 2017.
Health Populi’s Hot Points: So, Gregg and John, to your question: has patient empowerment and engagement scaled yet in U.S. healthcare?
Well, it depends on how we define the terms, and through what and whose lens. I do see green shoots of engagement among patients in the U.S., both for clinical activation and financial/shopping muscles.
A question in the Change Healthcare survey hints at one of the challenges in assessing and inspiring patient engagement: “What is the best approach for turning passive patients into active healthcare consumers?”
For many years, my discussions with patient activists on social media have informed me about some of the toxic language that prevents trusted conversations between people – patients, consumers, caregivers — and health care providers, plans, and pharma. Words like “adherence,” “compliance,” and in this question the verb, “turning,” are turn-offs for the very people legacy healthcare organizations want to engage.
Contemporary health engagement for patients in the U.S. is also complicated by the fact that patients are responsible for financing at least part of their healthcare — resulting in self-rationing among a large percentage of people who truly need to access care, the CarePayment survey points out. We’ve seen these behaviors based on other data sources, notably over the years via the Kaiser Family Foundation which I perennially cover — even back in 2012 before the advent of the Affordable Care Act.
As providers, payors and pharma allocate capital resources for technology to improve relationships with patients on the hardware side of the ledger, these healthcare organizations should also be mindful of other processes and mindsets facing consumer-patients — both in terms of helping people navigate the healthcare system, and at the same time, avoid the financial toxicity that can prevent them from seeking care in the first place.
The post Consumer Health and Patient Engagement – Are We There Yet? appeared first on HealthPopuli.com.
Consumer Health and Patient Engagement – Are We There Yet? posted first on http://drugsscreeningpage.blogspot.com/
No comments:
Post a Comment