 For this end-of-year post leading into 2018, I choose to address the big topic of how long we live in America, and what underpins the sobering fact that life expectancy is falling.
For this end-of-year post leading into 2018, I choose to address the big topic of how long we live in America, and what underpins the sobering fact that life expectancy is falling.
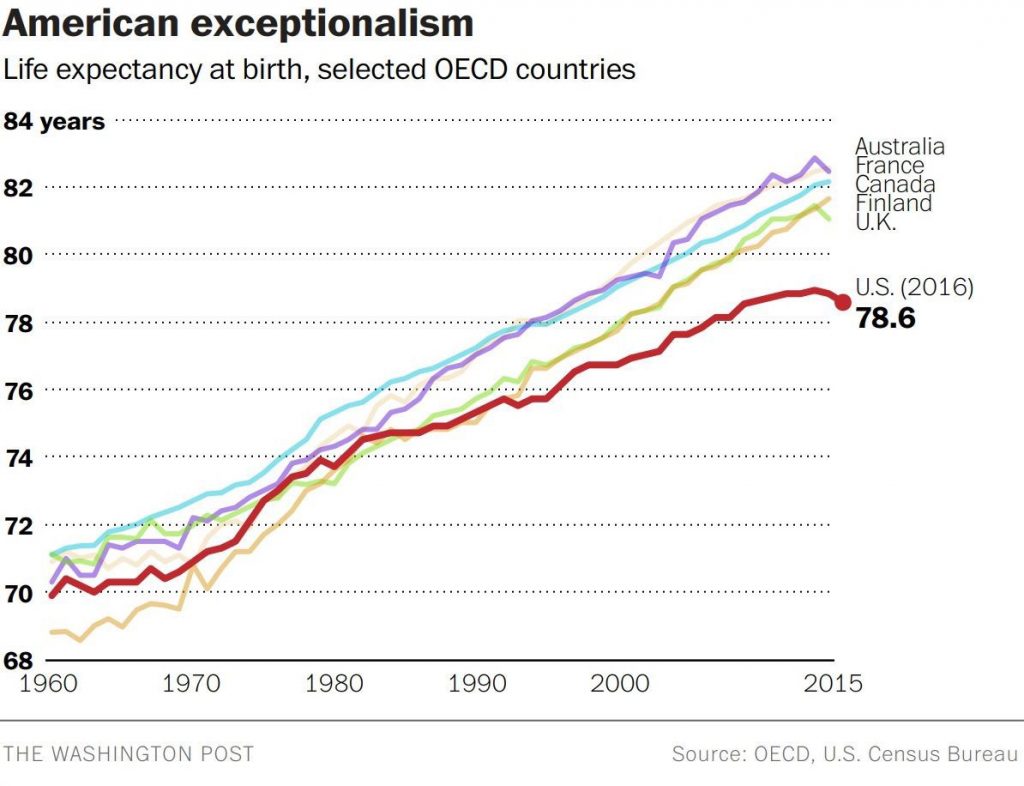
Life expectancy in the United States declined to 78.6 years in 2016, placing America at number 37 on the list of 137 countries the World Economic Forum (WEF) has ranked in their annual Global Competitiveness Report 2017-2018.
The first chart shows the declining years for Americans compared with health citizens of Australia, France, Canada, Finland, and the UK. While Australians’ and Britons’ life expectancies declined from 2015-16, their outcomes are still several years greater, at 82.5 for the Aussies (#10) and 81.6 for the Brits (#20).
The U.S. falls between #36, Qatar, and #38, Poland, in this analysis, below lower-income nations like South Korea (#12), Malta (#16), Chile (#18), and Slovenia (#29).
The WEF report talks about countries’ abilities to do business and mashes up dozens of data points, well beyond life expectancy. The Global Competitive Index is made up of factors covering institutions, infrastructure, macroeconomics, health and primary education, higher education and training, goods market efficiency, labor market efficiency, financial market development, technological readiness, market size, and innovation.
There are three sub-indexes that make up the big GCI: basic requirements, efficiency enhancers, and innovation and sophistication factors. Overall, the U.S. scores very high, #2, on the macro Global Competitive Index, just after Switzerland and before Singapore; good news, indeed, for business.
But you have to dive deep into the 393 page document, to page 326, to see the low performance of the U.S. in one specific sub-index which is what underlies America’s declining life expectancy and risk factors to living well: on the “basic requirements sub-index,” the U.S. garners the 25th spot on the list of 137.
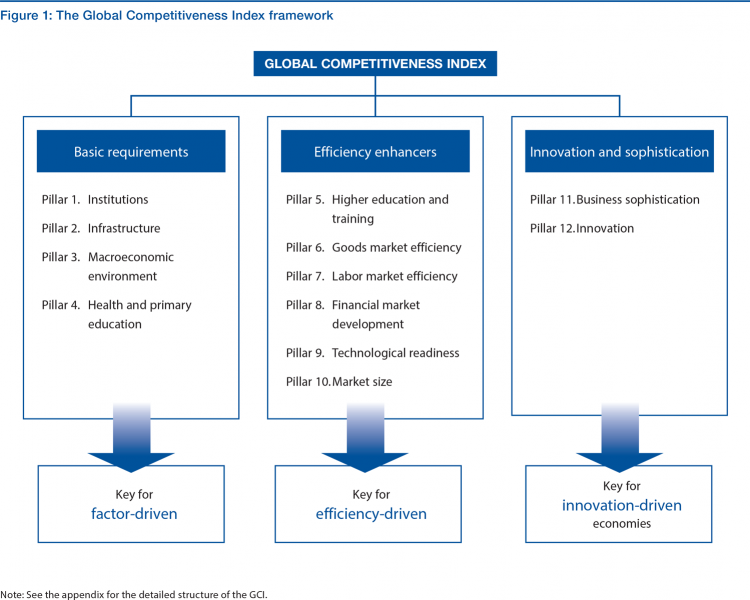 What comprises “basic requirements?” we’re begged to ask. These pillars are shown in the second diagram on the left third of the chart: they are institutions, infrastructure, macroeconomics, and health and primary education.
What comprises “basic requirements?” we’re begged to ask. These pillars are shown in the second diagram on the left third of the chart: they are institutions, infrastructure, macroeconomics, and health and primary education.
Most of the datapoints underneath these pillars are social determinants of health: beyond health and primary education, macroeconomics set the context for health citizens’ financial wellness, job and income security. Infrastructure can bolster or diminish public health through clean (or dirty) water, clean (or dirty) air, safe and healthy physical built environments, and accessible and active transportation networks.
The U.S. performance on basic requirements improved at the margin in 2016, with the macroeconomic environment at a low of 83 out of the 137 world nations.
Health Populi’s Hot Points: Thinking about the WEF “fine print” on basic requirements can help us understand what underlies declining life expectancy in the United States of America.
Most of the coverage of this statistic has been focused on the impact of the opioid epidemic in the U.S. A few others, rightly, point to obesity and the risk factors for non-communicable disease.

The U.S. is hardly “united” in this statistic: for people who live longer, it helps to be born and raised in a wealthier zip code, have access to better education and healthy food sources. A Lancet article published earlier this year, Inequality and the health-care system in the USA, noted that “widening economic inequality in the USA has been accompanied by increasing disparities in health outcomes.”
Overlay these new data from the U.S. Bureau of Economic Analysis (BEA) on personal consumption, credit card use, and declining savings rates among Americans. These stats were published on 22nd December 2017, so are current as of end-of-year 2017.
Americans’ personal income grew 3.8%, up from 1.5% a year ago. That sounds like good news; however, this was driven in major part by inflation, which increased in 2017 (blame that primarily on energy prices). Adjusted, people’s disposable personal income growth was only 0.88% after taxes and inflation.
Couple this with consumer spending, which may be topping out. Why? Because the personal savings rate in the U.S. hit a new low, falling to 2.9%, shown in the diagram. Based on this new low savings rate, consumers are turning more to credit to pay for consumption.
So credit card use is rising while personal saving is falling.
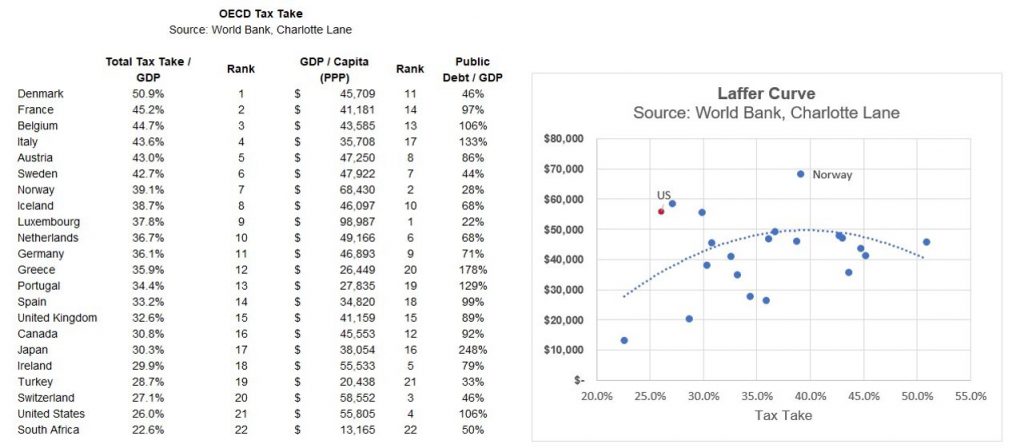 “The consumer is maxed out,” notes Eric Basmajian who so wisely parsed the BEA data. See this chart for which Eric arrayed the tax rates for OECD nations, from highest to lowest. Check out the U.S., second from the bottom, just above South Africa.
“The consumer is maxed out,” notes Eric Basmajian who so wisely parsed the BEA data. See this chart for which Eric arrayed the tax rates for OECD nations, from highest to lowest. Check out the U.S., second from the bottom, just above South Africa.
While income disparities continue to widen in the U.S., the Tax Cuts and Jobs Act signed by President Trump on 22nd December does not have as an explicit objective of redistribution of wealth from the very wealthy to the lowest-earning 20% of Americans.
Thus, the dramatic disparity between rich and not-so-rich, at the root-of-the-root of declining health in America, will persist into 2018.
Filter this personal economic data through a health care lens. Most Americans live paycheck to paycheck to make ends meet, a CareerBuilder survey learned earlier this year. Over one-half of Americans could not pay for a $400 emergency without borrowing money from someone or taking it out of their 401(k) retirement fund.
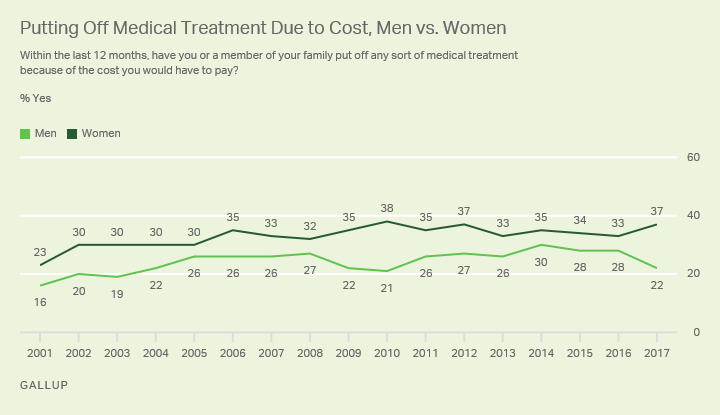
Gallup’s November 2017 poll on health care costs found that about one-third of Americans put off medical treatment due to costs, and more women (37%) than men (22%) do. This may be due to the fact that women’s healthcare costs are typically higher than men’s. What’s most somber about this statistic is that nearly two-thirds of people who forego care due to cost say they have a serious condition. Self-rationing of care due to cost can lead to earlier, avoidable, disability and death.
Let 2018 be a year when we value health, health care providers, and truth-telling so we can join together to help make America’s healthcare great again.
The post Let’s Increase Life Expectancy in America in 2018 – A New Year for Opioids, Social Determinants, and Financial Health appeared first on HealthPopuli.com.
Let’s Increase Life Expectancy in America in 2018 – A New Year for Opioids, Social Determinants, and Financial Health posted first on http://drugsscreeningpage.blogspot.com/
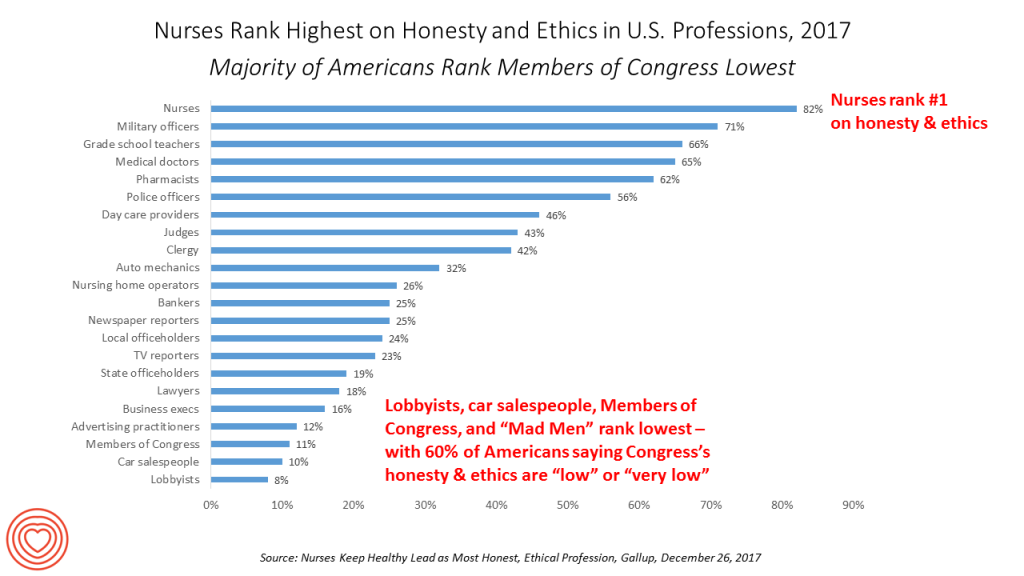 Nurses working in the U.S. are number one when it comes to ethics and honesty,
Nurses working in the U.S. are number one when it comes to ethics and honesty, 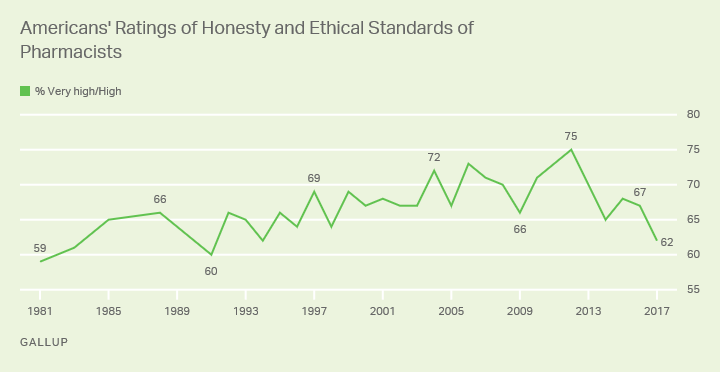
 MOIA is a brand and a self-described “social movement.” The organization’s objective is, “to develop and offer an extensive portfolio of on-demand mobility services that make the lives of people living in urban areas better, cleaner and safer.”
MOIA is a brand and a self-described “social movement.” The organization’s objective is, “to develop and offer an extensive portfolio of on-demand mobility services that make the lives of people living in urban areas better, cleaner and safer.”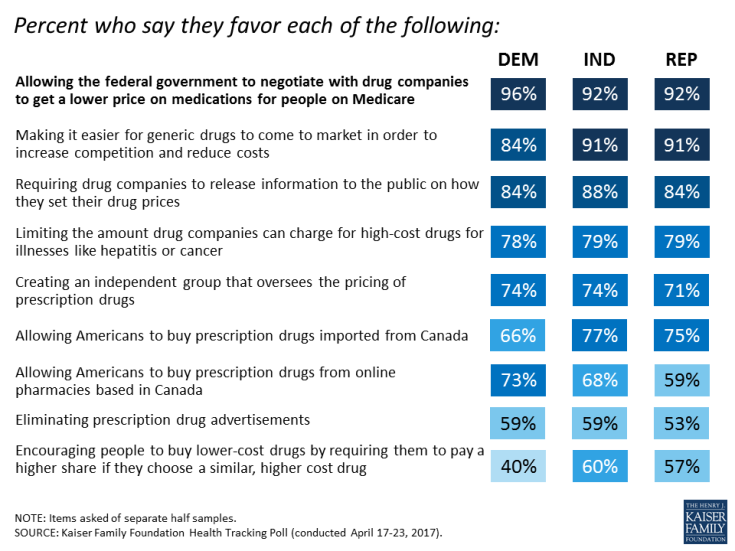 Because consumers have a retail relationship with prescription drugs through pharmacies, the issue gets peoples’ attention due to greater price transparency – at least in the form of co-pay, coinsurance, or first-dollar payment under a high-deductible health plan. Pharmacies understand their role as accessible retail health on-ramps for medications and counsel, and growing role as health care providers. In 2017, CVS launched a drive-up service for consumers to collect their prescriptions at the curbside. Then the company announced intentions to deliver Rx to patients’ homes. Finally,
Because consumers have a retail relationship with prescription drugs through pharmacies, the issue gets peoples’ attention due to greater price transparency – at least in the form of co-pay, coinsurance, or first-dollar payment under a high-deductible health plan. Pharmacies understand their role as accessible retail health on-ramps for medications and counsel, and growing role as health care providers. In 2017, CVS launched a drive-up service for consumers to collect their prescriptions at the curbside. Then the company announced intentions to deliver Rx to patients’ homes. Finally, 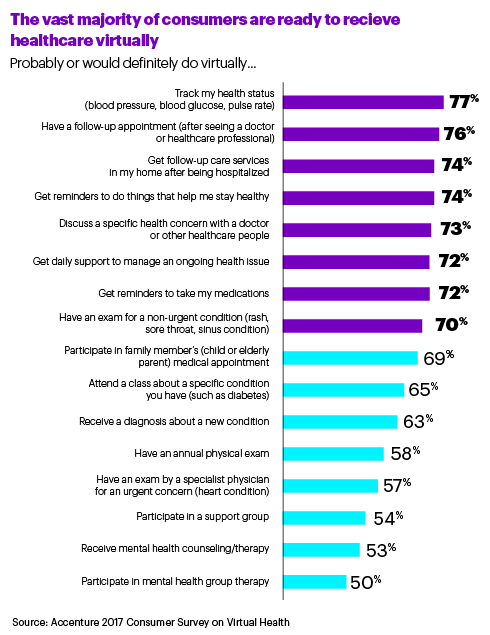 Consumers’ interest in virtual and telehealth will grow in 2018:
Consumers’ interest in virtual and telehealth will grow in 2018: 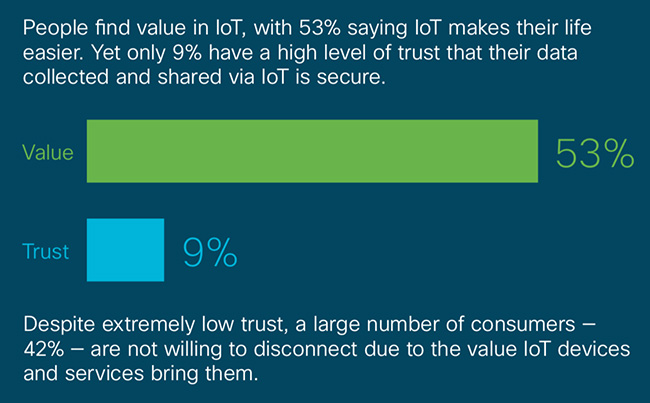 But people have
But people have 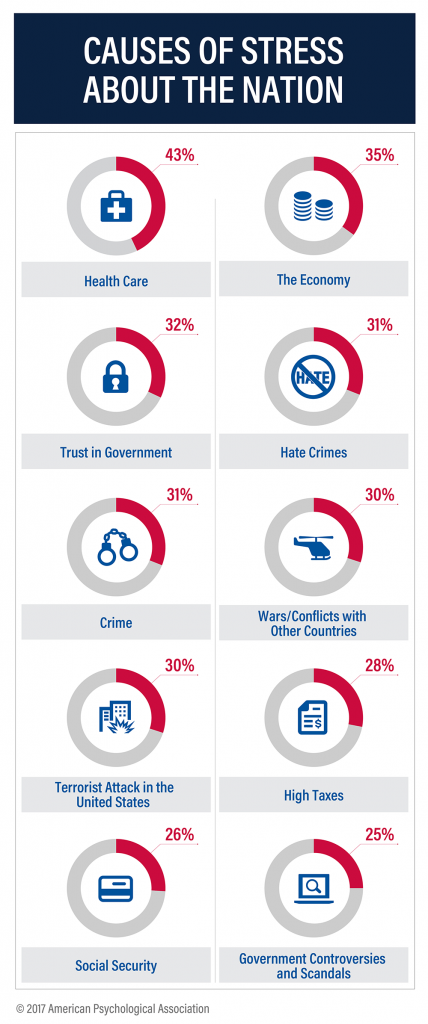 Why growing attention to self-care among U.S. healthcare consumers? It’s to feel better and manage healthcare costs, for sure, but there’s another factor: other people. 53% of Americans are engaging in better self-care to be better for others, Field Agent’s poll found.
Why growing attention to self-care among U.S. healthcare consumers? It’s to feel better and manage healthcare costs, for sure, but there’s another factor: other people. 53% of Americans are engaging in better self-care to be better for others, Field Agent’s poll found. The concern from advocates to keep net neutrality is that the large ISPs — AT&T, Comcast, and Verizon, among them — could be so-called “bad actors” in favoring fast-lane communications for certain content versus other information that consumers, under net neutrality, could access equally. Ultimately, “could ISPs become content-controllers, or charge additional ‘tolls?” those who wish to preserve net neutrality have asked.
The concern from advocates to keep net neutrality is that the large ISPs — AT&T, Comcast, and Verizon, among them — could be so-called “bad actors” in favoring fast-lane communications for certain content versus other information that consumers, under net neutrality, could access equally. Ultimately, “could ISPs become content-controllers, or charge additional ‘tolls?” those who wish to preserve net neutrality have asked.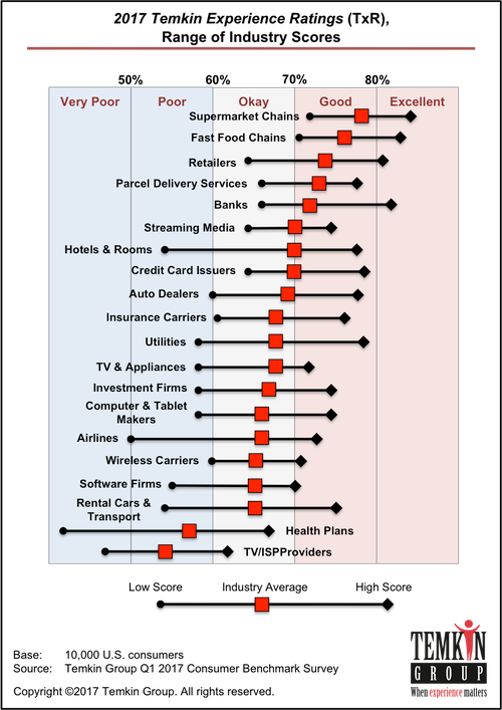 Interestingly enough, consumers ‘get’ that ISPs haven’t delivered on customer service, we know from
Interestingly enough, consumers ‘get’ that ISPs haven’t delivered on customer service, we know from 
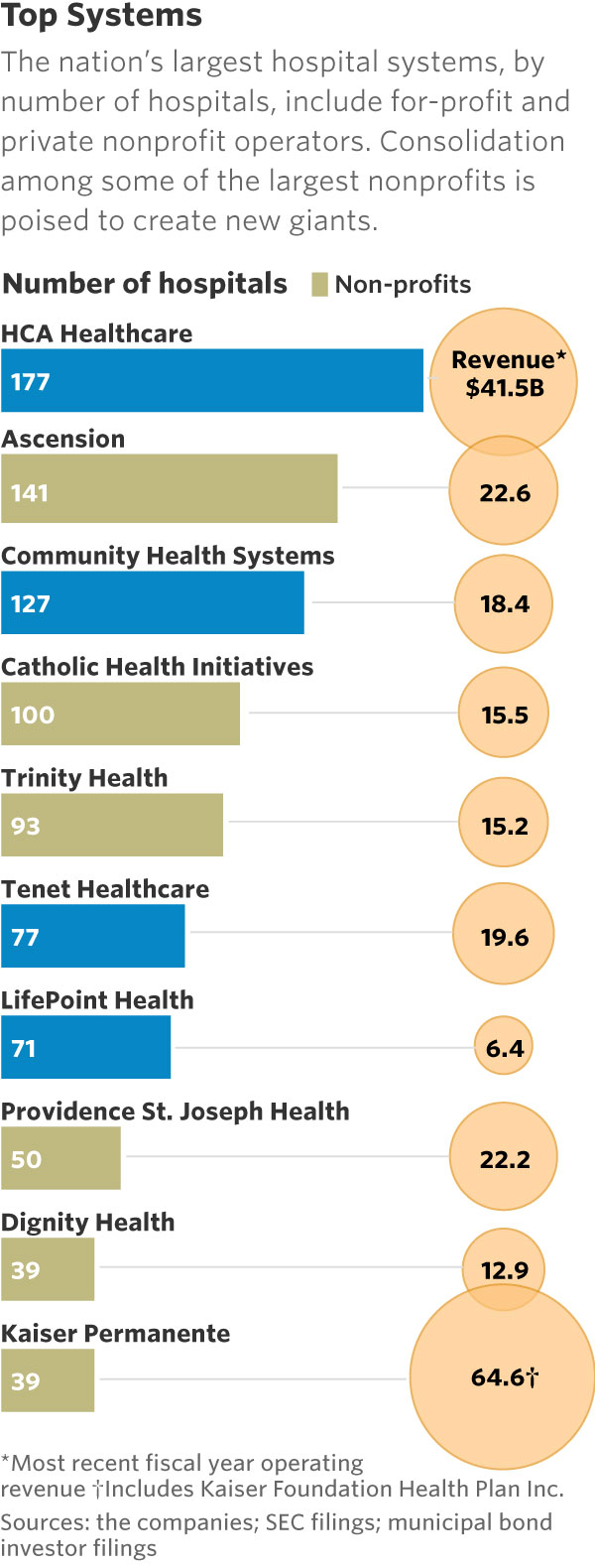 This month, two hospital mega-mergers were announced between
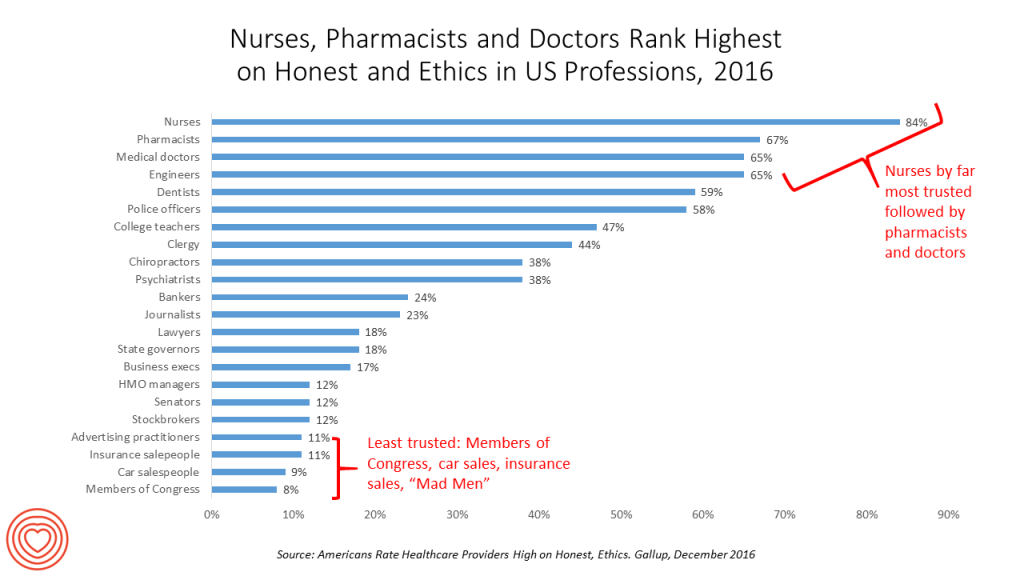
This month, two hospital mega-mergers were announced between 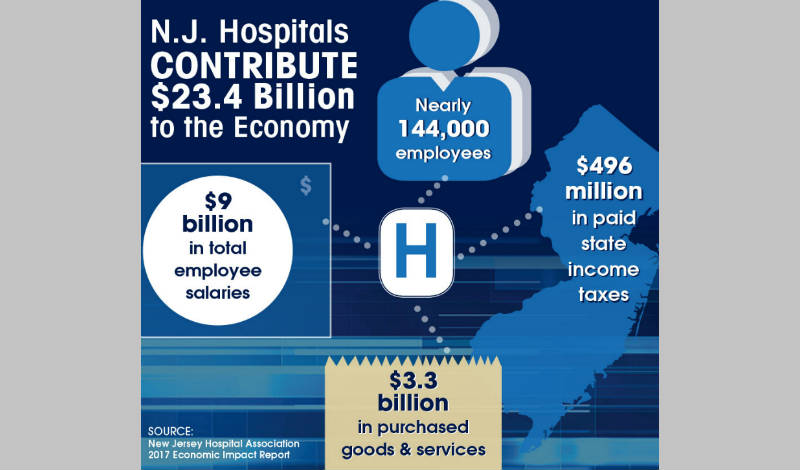 Hospitals should be mindful that trust is necessary for patient/health engagement. And the trust is with hospitals if the organization chooses to leverage that goodwill for a value-exchange. Hospitals are economic engines in their local communities — often, the largest employer in town. “Everyone” in most communities knows someone who works in a hospital.
Hospitals should be mindful that trust is necessary for patient/health engagement. And the trust is with hospitals if the organization chooses to leverage that goodwill for a value-exchange. Hospitals are economic engines in their local communities — often, the largest employer in town. “Everyone” in most communities knows someone who works in a hospital. As Mufasa told Simba in The Lion King, “You are more than what you have become. Remember who you are.”
As Mufasa told Simba in The Lion King, “You are more than what you have become. Remember who you are.”